An important protective function of the body is the formation of blood clots with the help of platelets and fibrin, which, when the vessels are damaged, prevent blood loss. This is the process of coagulation, for which the homeostasis system is responsible. Deep vein thrombosis: symptoms and treatment
But sometimes coagulation is not good but becomes a serious pathology. The formation of a blood clot without damage to the vessel leads to the fact that a clot – embolus begins to wander around the bloodstream. It blocks the lumen of the vein and clogs it, which leads to thrombosis. The blockage of a blood vessel causes circulatory disturbance and an inadequate supply of organs. In the case of complete overlap of the lumen of the vessel, hypoxia develops, due to which the death of cells begins.
The main danger of the disease is frequent suddenness. In a person who has almost no suspicion, a blood clot comes off and thromboembolism (blockage) of the pulmonary arteries develops and then the chances of timely help and a successful outcome are quite small.
Localization thrombosis can be venous and arterial. Venous, in turn, is divided into thrombophlebitis of superficial veins and deep vein thrombosis. According to statistics, superficial veins account for more than 90 percent of thrombosis, and deep veins – 5-10 percent. Deep vein thrombosis (DVT) will be discussed in more detail in this material. Deep vein thrombosis: symptoms and treatment
Table of Contents
- What is deep vein thrombosis?
- Acute Deep Vein Thrombosis
- Causes of Deep Vein Thrombosis
- Congenital Risk Factors
- Acquired Risk Factors
- Mixed risk factors
- Signs and symptoms of Deep Vein Thrombosis
- If the temperature of the foot rises
- Diagnostics
- Thrombosis treatment
- Drug treatment
- Surgery
- Is thrombosis treated forever
- Complications
- Rehabilitation after DVT
- DVT Prevention
What is deep vein thrombosis?
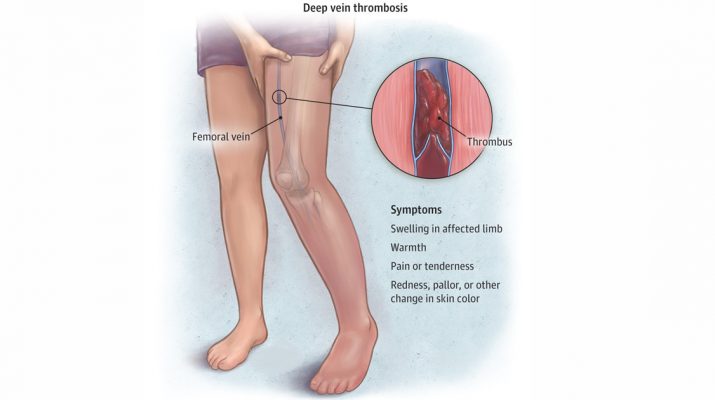
Deep veins are called that are invisible when examined. They are located in the intramuscular fascial canals and divert blood from groups of deep muscles. Deep vein thrombosis of the lower extremities is the formation of a thrombus in these vessels and the subsequent deterioration of blood flow.
With deep vein thrombosis, blood can reach the heart only through small vessels, which is why swelling and an increase in the temperature of the limb, in which the problem develops, form at the site of vein obstruction.
There are several classifications of pathology. The main ones are:
- by localization;
- at the stage of development;
- on etiology;
- according to the clinical course.
According to the localization, DVT is divided into segments in which the problem develops:
| Segment | Affected Deep Veins |
| Lower | Trunk veins of the lower extremities. |
| Average | External and general iliac veins. |
| Upper | Inferior vena cava. |
The disease often develops in these vessels. With its development in other deep veins, pathology is attributed to the segment in which it is located.
Deep vein thrombosis develops in three stages:
- acute – up to one month;
- subacute – after completion of acute and up to three months;
- chronic – after three months from the onset of the disease.
Acute Deep Vein Thrombosis
The most dangerous stage of the disease is acute. In the period up to one month from the moment of the onset of the disease, all therapeutic actions must be taken to stop the disease and eliminate the risk of complications.
If you miss the moment for a drug intervention, then the transition to the subacute stage will not occur.Deep vein thrombosis will provoke complications that can lead to death
It is important to correctly diagnose the disease at the time of its inception. This will leave time for choosing the right treatment tactics and preventing complications.
By etiology, deep vein thrombosis of the lower extremities can be:
- primary,
- congenital.
In the clinical course, the compensation stage and the decompensation stage are distinguished. A single classification system for deep vein thrombosis does not exist. In total, there are more than twenty options for sharing this diagnosis. These are the most common.Deep vein thrombosis: symptoms and treatment
Causes of Deep Vein Thrombosis
The main pathogenetic causes of thrombosis are three:
- damage to the walls of the vein,
- impaired blood flow
- violation of the blood.
These are direct causes of vascular thrombosis. And they are caused by a number of reasons that are attributed to risk factors for the development of leg thrombosis. They are divided into three groups:
- congenital
- acquired
- mixed.
Congenital Risk Factors
Congenital or genetic risk factors are the characteristics of the body of a particular person, because of which he increases the likelihood of blood clots. The factors of this group include:
- antithrombin deficiency – a substance that inhibits the process of blood coagulation;
- problems with the homeostasis system;
- congenital pathologies of the circulatory system;
- problems with the secretion and absorption of proteins C and S.
Congenital factors are the most dangerous. They are practically not diagnosed without visible manifestations and can be manifested immediately by problems with blood circulation.
Acquired Risk Factors
This group includes acquired diseases, bad habits and associated risk factors for thrombosis.
The most common risk factors for deep vein thrombosis are given in the table:
| Risk factor | Frequency encountered |
| High blood pressure (hypertension) | 75% |
| Phlebeurysm | 62% |
| Chronic obesity | 56% |
| Atherosclerosis | 44% |
| Diabetes | 37% |
| Smoking | 21% |
These figures are taken from a study by specialists of the Gomel State Medical University. In addition to these reasons, the risk factors for deep vein thrombosis are:
- chronic lung disease;
- fractures in the lower leg;
- the presence of a catheter in the central vein;
- liver pathology;
- heart attack before the age of 45 years;
- general anesthesia;
- surgical intervention on the bones;
- oncological diseases ;
- use of oral contraceptives.
Mixed risk factors
In this group, factors associated with blood coagulation: high levels of homocysteine (an amino acid that provokes the formation of blood clots and atherosclerotic plaques) and fibrinogen (a protein dissolved in blood plasma).Deep vein thrombosis: symptoms and treatment
Signs and symptoms of Deep Vein Thrombosis
Deep vein thrombosis has several specific symptoms, but it can be asymptomatic. Circulatory problems are indicated by:
- severe swelling at the site of occlusion of the vessel;
- discoloration of the skin, often throughout the limb;
- unexpressed pain, which intensifies with a load on the legs;
- significantly warmer or hotter leg with thrombosis (hyperthermia).
Cases of asymptomatic course are more dangerous. Due to untimely treatment, the disease can flow into serious complications, causing irreversible consequences.Deep vein thrombosis: symptoms and treatment
If the temperature of the foot rises
One of the most striking signs of the rapid development or complication of deep vein thrombosis is local hyperemia. It is impossible to accurately measure the temperature of the leg, but it is tactile to feel that one limb is warmer than the other. This symptom is a reason for immediate hospitalization, so as not to miss further complications, in particular, pulmonary embolism.
Diagnostics
Diagnosed with deep vein thrombosis by a complex of methods. At the first stage, the doctor collects the patient’s history, which collects data on the presence of the development factors of the disease: congenital, acquired and mixed.
At the second stage, the patient is examined, a blood test and a coagulogram. These studies should capture the visual signs of deep vein thrombosis, demonstrate indicators of blood coagulation and its characteristics.
The third stage – an instrumental examination, is carried out to clarify the diagnosis and determine the nature of the disease.
The basis of instrumental diagnosis of deep vein thrombosis is ultrasound duplex scanning of veins. This method evaluates the basic hemodynamic parameters and reveals structural changes in the walls of blood vessels.
The procedure is lengthy, but only it shows the presence of several pathologies, including deep vein thrombosis. If ultrasound duplex scanning of veins is not possible, the disease is diagnosed by other methods:
- multispiral computed tomography;
- MRI angiography.
The choice of diagnostic method remains with the doctor.
Thrombosis treatment
Treatment is selected depending on each specific case. There are two main treatment options for thrombosis:
- medication
- surgical
Drug treatment is the most common way to treat leg thrombosis. Most often it is used independently. If surgical intervention is necessary, concomitant therapy is medication.
The therapy of deep vein thrombosis should solve five problems:
- decreased thrombus growth;
- an exception to the development of pulmonary embolism;
- prevention of venous gangrene by combating swelling;
- restoration of the lumen of the vessel;
- recurrent prophylaxis.
Drug treatment
A patient with diagnosed deep vein thrombosis is placed in a hospital, in the surgical or, if available, angio surgery unit. Strict bed rest is necessary for the patient until the pronounced swelling is eliminated and the risk of developing floating thrombosis is eliminated. Drug therapy for DVT is based on drugs from four groups:
| Drug group | Description |
| Anticoagulants | The main group of drugs for thrombosis. Used to reduce blood coagulation and prevent the development of blood clots. |
| Antiplatelet agents | A group of drugs to prevent the development of blood clots. Reduces the ability of platelets and red blood cells to adhere to the endothelium of blood vessels. |
| Nonsteroidal anti-inflammatory drugs | Medicines to relieve the main symptoms of DVT: an inflammatory reaction of the venous wall and pain manifestations. |
| Phleboactive drugs | Medications to improve venous and lymphatic blood flow. Increase the tone of the venous walls and relieve swelling. |
Antibiotics for deep vein thrombosis are rarely used. Indications for their appointment:
- high risk of septic complications;
- pustular skin lesions.
Anticoagulants are the most effective group of drugs for the treatment of deep vein thrombosis. The result of their action is one: a decrease in coagulability. But according to the mechanism of its achievement, anticoagulants are:
- straight
- indirect.
Direct anticoagulants directly interfere with the coagulation process, inhibiting one of its factors. The most common coagulant – heparin, interferes with the operation of thrombin.
Indirect coagulants do not directly affect blood coagulation factors. They inhibit the synthesis of substances that are involved in coagulation. At the first stage of DVT treatment, direct anticoagulants are prescribed, most often heparin. Its dose and duration of therapy depend on a number of factors, the main of which is temporary indicators of blood coagulation.Deep vein thrombosis: symptoms and treatment
In the second stage, direct anticoagulants are replaced by indirect ones. During the transition, it is necessary to take drugs of both groups at the same time, for three to four days.
The duration of drug therapy for thrombosis is from three months to six months since during this period, relapse is possible.
Surgery
The most common method for surgical treatment of deep vein thrombosis is to install a cava filter, a small tool for filtering blood flow and trapping blood clots.
This method is one of the most effective in preventing the development of pulmonary embolism. A cava filter is inserted into the inferior vena cava using a catheter. It does not interfere with natural blood flow, but effectively traps blood clots. Kava filters are temporary and permanent, the choice of a particular one depends on the characteristics of the patient.
A filter element is placed under local anesthesia in departments with a vascular specification. The procedure itself, nominally, is not complicated, but it requires a set of equipment and several specialists, including an anesthetist.
There are also other surgical treatments for DVT:
- thrombectomy
- plication
- ligation of the main veins.
Thrombectomy is a surgical procedure to remove a blood clot. During thrombectomy, an incision is made in the vessel at the site of the formation of the thrombus and it is removed with a special tool. Thrombectomy is the most effective and radical way to treat thrombosis.
Variants are also possible when a portion of the affected vessel is removed during thrombectomy. This method is outdated, but it is still used in severe cases of the disease.
The inferior vena cava plication is an operation to organize natural blood filtration from large thromboembolism. During plication, the lumen of the vessel with metal brackets is divided into several small channels. This does not slow down the blood flow but prevents blood clots from moving through the bloodstream.
Plication is an alternative to installing a cava filter when its integration into a vessel is not possible.
Ligation of the main veins is one of the oldest ways to prevent pulmonary embolism. Only the vein is bandaged above the site of the formation of the thrombus, the violation of the blood flow through which will not cause critical dysfunction of the venous outflow.
In terms of effectiveness, dressing is one of the best methods, but it is rarely used now because of many contraindications and the presence of less traumatic treatments for DVT.
Is thrombosis treated forever
The issue of full recovery after deep vein thrombosis should be considered in two planes. If you look at the treatment of the manifestations of the disease, then yes – the disease can be cured: remove the thrombus by surgery or medication.
But if you look more globally, then it is impossible to completely get rid of the likelihood of developing a disease. This is especially true for people who have congenital risk factors for the disease.
They can be corrected, suppress their effect on the circulatory system, reduce the likelihood of developing the disease, but you can not completely get rid of them. This does not mean that with congenital risk factors, a person’s life turns into a constant struggle. But he needs constant preventive measures that reduce the risk of developing the disease.
Prevention is important to everyone. Even the absence of congenital risk factors does not allow us to be sure that DVT will not affect a person. Indeed, with the acquired factors, some can be excluded, but some can not be controlled. They can occur regardless of behavior and lifestyle.
One thing is certain with certainty: an effective therapy for the problem exists, with timely diagnosis, the risk of developing irreparable consequences is minimal. But everyone should independently reduce the risk of the disease: due to the timely treatment of provoking pathologies, due to the rejection of bad habits, due to proper nutrition.
Such steps are much more important than clinical treatment, since they prevent the occurrence of the disease.
Complications
The main complication of deep vein thrombosis is post-thrombophlebitis. She is a direct consequence of the treatment of the disease. The mechanism of its development is the violations that occur in the bloodstream after the removal of blood clots. In its place appears connective tissue, which cannot work as the natural wall of the vessel.
This leads to an increase in pressure in the blood vessels, destruction of the valves and a general violation of the blood flow. Post-thrombophlebitis disease is a serious complication of DVT, which requires full-fledged drug therapy.
A doctor who monitors the patient’s rehabilitation after thrombosis can accurately determine the onset of the disease according to the patient’s complaints and a simple examination. Therefore, the completed treatment of deep vein thrombosis is the best prevention of its complications.
In the initial stages, complications are easier to stop, and their prevention gives good results.Deep vein thrombosis: symptoms and treatment
Rehabilitation after DVT
Rehabilitation of patients after deep vein thrombosis is needed to solve three problems:
- prevention of re-development of the disease;
- prevention of the development of post-thrombophlebitis disease;
- compensation of venous outflow.
The main methods of the rehabilitation program:
- regular motor activity;
- time limit of static vertical stay of the body;
- the use of compression hosiery.
Doctors emphasize that without a rehabilitation program it is impossible to talk about a complete victory over deep vein thrombosis.
DVT Prevention
Preventive measures to reduce the risk of deep vein thrombosis are measures to improve blood flow in the lower extremities and to reduce the likelihood of blood clots. For a person with a history of neither congenital nor acquired risk factors, DVT prophylaxis is:
- regular physical activity;
- lack of prolonged immobilization;
- a sufficient amount of fluid in the diet;
- wearing comfortable shoes;
- lack of static loads on the legs.
This list is expanding as one of the risk factors a person has. One of the most effective methods of prevention is the use of compression stockings.
The squeezing such knitwear exerts helps maintain an adequate state of blood flow. As a result of full-fledged blood movement through deep veins, the tendency of blood to form blood clots decreases.
Such stockings are widespread in people with varicose veins and in those who have to fly a lot. At altitude, the air pressure is lower and the pressure created by the compression hosiery compensates for it.
Studies show that in-flight compression stockings eliminate the risk of developing DVT and reduce swelling. At the moment, this is the most effective prevention method for people with DVT risk factors.
We must not forget about a healthy lifestyle. Smoking, alcohol, malnutrition – all these factors contribute to the formation of blood clots. If excluded, the risk of thrombosis will decrease dramatically.