Few things are scarier than a strange lump somewhere on your body. That said, most lumps, as skin anomalies, tend to be rather harmless in nature. However, given the serious nature of certain medical conditions associated with lumps, we should possess at least a rudimentary understanding of these occurrences.
If You Do Find A Lump Somewhere On Your Neck, Here Are A Few Potential Reasons Why:
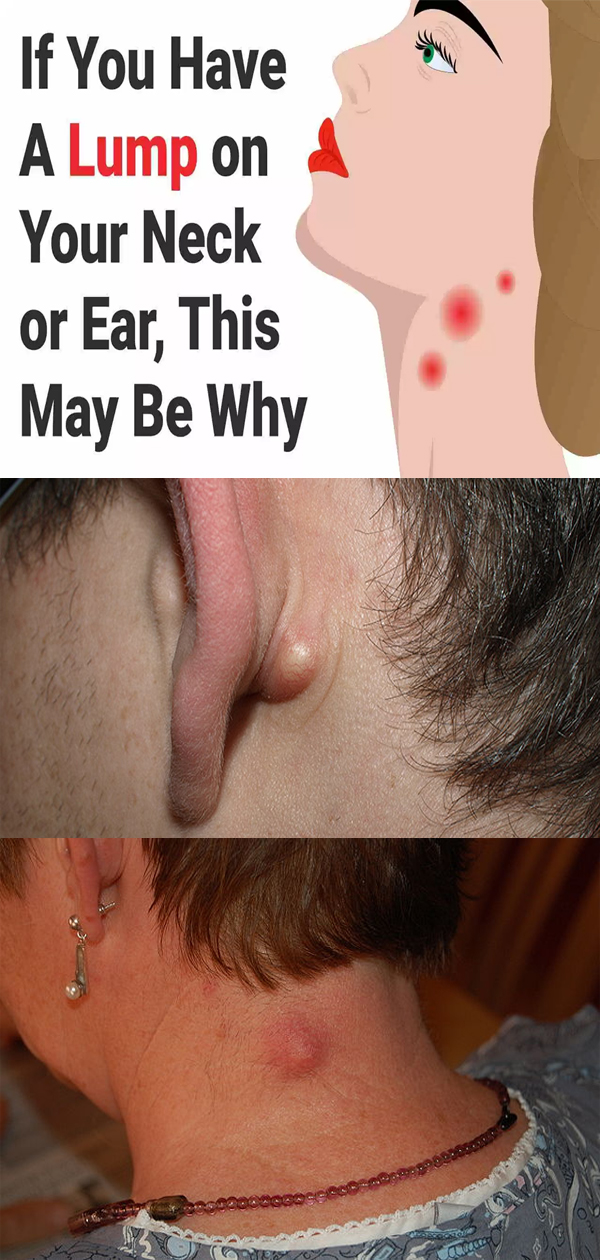
1. Swollen Lymph Nodes (Neck Or Ear)
Lymph nodes are slight structures that act as a filter, identifying and draining harmful substances from the body. The lymph nodes contain immune cells capable of neutralizing germs that cause illness and infection.
Swollen (or “enlarged”) lymph nodes is the most common cause of lumps appearing on the neck. Swollen lymph nodes are not always visible as they can be tiny, rarely exceeding the size of a pea.
In other parts of the body, the leading cause of swollen lymph nodes is the Epstein-Barr Virus (EPV), which is spread via saliva. For swollen nodes in the neck, ear infections are the most common trigger.
Children who contract swollen lymph modes may develop a white, pus-like substance on the tonsils. Symptoms of the condition include bean-sized lumps around and under the jaw or sides of the neck; and pain, swelling, and tenderness around the affected area. Swollen lymph nodes are usually diagnosed by physical examination. The physician may also order a biopsy or x-ray imaging.
Associated symptoms usually last for three to four weeks. Conventional treatment includes bed rest and over-the-counter antibiotics such as aspirin, acetaminophen, and ibuprofen. Warm compresses applied to swollen areas can help alleviate pain and tenderness.
2. Infectious Mononucleosis (Neck)
Infectious mononucleosis (IM), more commonly referred to as “mono” or glandular fever, is an infection that produces swollen lymph nodes in the neck. As the name indicates, IM is an infectious disease that is spread via saliva. Most children are infected by IM at some point, in which case the illness causes few or no symptoms. Adulthood IM may produce symptoms that resemble the flu: body aches, fatigue, fever, headaches, night sweats, and sore throat.
In rare cases, complications from IM may arise, including obstruction of the airways, anemia, encephalitis, jaundice, and thrombocytopenia (low levels of blood platelets).
A serologic test – a type of blood test that measures antibody levels in the blood – is often used to diagnose mono. The presence of immunoglobin M (IgM) is indicative of a current mono infection. Mono may last anywhere from 3-4 weeks and is treated by OTC antibiotics and bed rest.
3. Goiter (Neck)
Goiter is an abnormal enlargement of the thyroid gland – a butterfly-shaped gland surrounding both sides of your neck directly underneath your Adam’s apple. It often appears as a large “bubble” – a mass on one or both sides of the neck.
In many places, particularly underdeveloped countries, goiter is predominantly caused by a lack of iodine in the diet. The most common cause in countries such as the U.S. is underproduction or overproduction of thyroid hormone – hypothyroidism and hyperthyroidism, respectively. The growth of small lumps called nodules may lead to goiter. Hormonal complications resulting from inflammation or pregnancy are other causes.
Some goiters are non-symptomatic. For those that do produce symptoms, the most common are visible swelling, coughing, difficulty breathing, difficulty swallowing, hoarseness, and a feeling of throat constriction. Too much or too little thyroid hormone may produce symptoms such as fatigue, irritability, insomnia, and weight gain (or loss).
Goiter is diagnosed by one or more of the following: physical examination, hormone test, ultrasound, thyroid scan, and biopsy. If needed, treatment may involve medication, surgery, or a combination of both. Depending on the goiter’s size and side effects, your doctor may opt for a wait-and-see approach with regular office visits.
4. Sebaceous Cyst (Neck Or Ear)
A sebaceous cyst is a skin abnormality that arises from the sebaceous gland. The sebaceous gland is a microscopic subdermal structure surrounding the hair follicles that secretes oil and wax. It is responsible for lubricating and waterproofing the hair and skin.
The cysts vary in size and are usually round in shape. Sebaceous cysts consist of keratin – a structural protein – and fibrous tissues and fluids. Keratin resembles cottage cheese in texture and may give off a foot-odor-like smell. Sebaceous cysts are non-cancerous though they may be uncomfortable.
Sebaceous cysts may be caused by swelling of a hair follicle, elevated testosterone levels, and the use of anabolic steroids. Most sebaceous cysts do not require treatment by a doctor. If the doctor elects to have the cyst removed, the following procedure takes place:
- Numbing: local anesthesia applied to affected area
- Cleaning: use of antiseptics designed to avoid spreading infection
- Removal; use of a surgical instrument (e.g. scalpel) to detach and remove the cyst
If the area underneath the cyst is infected, the physician may drain the area and prescribe a course of antibiotics.
5. Abscess (Neck Or Ear)
Skin abscesses develop when the skin cells or tissue become infected. To counter the infection, the body transports white blood cells (WBCs) to the affected area. WBCs accumulate to the point that pus – a fluid consisting of skin components, bacteria, and dead WBCs – begins to form underneath the skin. Skin abscesses vary in texture and appearance, though they typically resemble a large pimple. Over time, the “head” begins to fill with fluid.
Staphylococcus is the most common reason for skin abscesses. “Staph” enters the body through a hair follicle, or through an injury or wound that has broken the skin. One can minimize the odds of staph infection by regularly washing hands, cleaning all skin cuts with soap and water, and bandaging all open wounds.
Individuals most at-risk for the development of skin abscesses include children, seniors, those with a weak immune system, recipients of organ transplants, and those undergoing cancer treatment. Prompt treatment for these demographics is essential to avoid further health complications stemming from the condition.
Symptoms of skin abscess may include fluid drainage from the affected area, skin lesions, skin inflammation, pain around the affected area, chills, fever, nausea, and swelling.
Diagnosis of an abscess includes a review of medical history and a physical examination of the abscess. If determined necessary, your doctor may collect sample fluid from the abscess to test for bacteria. Treatment options include home remedies (especially use of a warm compress), drainage, and antibiotics.
6. Skin Cancer (Neck, Ear, And Various Areas Of The Body)
Skin cancer is the proliferation of abnormal skin cells, causing genetic defects, mutations, and tumor growth. Detected early, the survival rate for Americans is near 99 percent. It is estimated that one in five Americans develops skin cancer by age 70.
The most common type of dangerous skin cancer is melanoma, which produces moles that are large and that appear strange in both color and shape. Perhaps the most obvious outward sign of skin cancer is skin growths that get larger over time and sores that do not heal.
Skin cancer can develop early in life through excessive sun exposure and the development of sunburn blisters – all before the age of 18. Other common causes include scarring from burns or disease, exposure to chemicals, and exposure to x-rays.
The three main types of skin cancer – melanoma, basal cell carcinoma, and squamous cell carcinoma – often take on different appearances. Melanoma appears as a new or existing spot that changes in color, shape, or size. Many are red or pink, and some are brown or black in coloration. Basal cell carcinoma appears red, dry, and scaly. Squamous cell carcinoma appears patchy, raised, and may eventually bleed.
Skin cancer treatment depends on the stage. Most cancers are detected and treated before they begin to spread. In early stages, surgical excision and removal of localized tumors are performed. Topical application of chemotherapeutic agents may be prescribed. In rare instances when cancer has spread, chemotherapy and radiation may be recommended.
Final Thoughts: Identifying Lumps And When To See A Doctor
Here is a quick guide for checking for the most common causes of bumps on the ears or the neck. You will need to touch the affected area, so please be sure to wash your hands prior to the self-check thoroughly.
Self-check
(1) Does the lump feel soft and flexible? If yes, the lump is likely a lipoma – a knot of fatty tissue that is usually harmless and goes away on its own.
(2) Does touching the lump cause pain? Is the area around the lump tender? If yes, the lump is probably a pimple or abscess.
(3) Do you experience any other symptoms such as chills, fever, or nausea? If yes, schedule a doctor’s appointment as these are typically signs of an infection. Should your symptoms quickly worsen, go to the emergency room.
(4) Does the lump appear to grow in size or doesn’t fully heal? If yes, schedule a doctor’s appointment. These are typical signs of melanoma.
A good rule of thumb besides this basic framework is to see a doctor whenever you are unsure. When it comes to your health, being safe is always better than sorry!